OCUA Concussion Recognition and Management Protocol

Adapted from: Parachute. (2017). Canadian Guideline on Concussion in Sport. www.parachutecanada.org/guideline
The Ottawa-Carleton Ultimate Association has developed the OCUA Concussion Protocol to help guide the management of athletes who may have a suspected concussion as a result of participation in activities in and around the sport of Ultimate. This protocol should be used by all individuals who interact with athletes inside and outside the context of Ultimate-related activities in Ottawa, including athletes, parents, coaches, officials, teachers, trainers, and licensed healthcare professionals.
Pre-Season Education:
It is important that prior to commencing a season of Ultimate that all athletes, coaches, parents, teachers, trainers and health professionals be familiar with the information found in the concussion recognition tool 5.
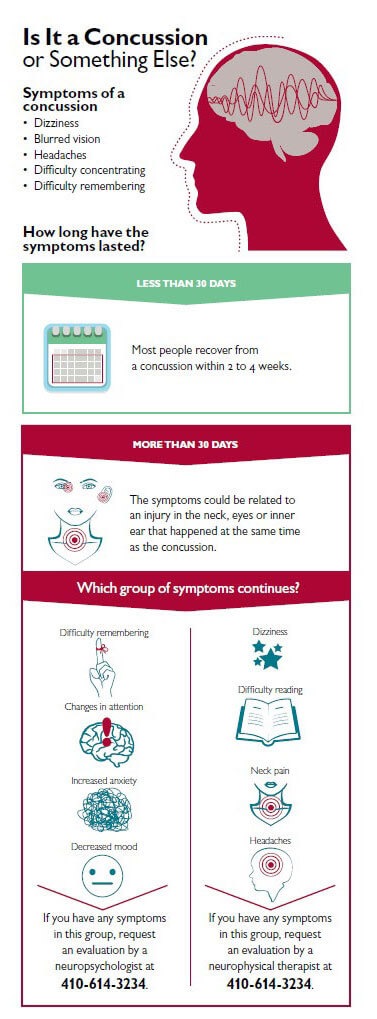
What is a concussion?
A concussion is a brain injury that cannot be seen on routine X-rays, CT scans, or MRIs. It affects the way a person may think and remember things, and can cause a variety of symptoms. Any blow to the head, face or neck, or a blow to the body which causes a sudden jarring of the head may cause a concussion. This can be a body collision, a hit to the head from an elbow or disc or hitting your head on the ground.
Concussion should be suspected in the presence of any one or more of the following:
- Symptoms (such as headache)
- Impaired brain function (e.g. confusion)
- Physical signs (such as unsteadiness)
- Abnormal behavior
What to do if you think a concussion has just occurred?
 When in doubt… sit them out!
When in doubt… sit them out!
Never return to play if you suspect concussive blow has occurred. Symptoms from a concussive blow may not appear until 5-7 days later and as such any player suspected of having a concussion should be removed from game play/practice until they have been medically evaluated. It’s better to wait one week than to rush back to sport. Do not be influenced by factors such as games where your team is missing players, finals etc.
How do I know if they need to go to the emergency room at a hospital?
If any of the following signs of symptoms have occurred following an injury to the head, neck or face, STOP, do not move the player unless they are in danger of further injury and seek immediate emergency medical assistance (call 911 or an ambulance):
- Neck pain or tenderness, Possible spine injury, skull fracture or bleeding
- Double vision
- Any loss of consciousness or deteriorating consciousness (unresponsive)
- Irregular heart rate, breathing, blood pressure
- Weakness, tingling or burning in the arms or legs.
- Severe or increasing headache
- Seizure or convulsion
- Loss of consciousness or deteriorating consciousness (unresponsive)
- Repeated vomiting
- Increasing restlessness, agitation or combative behavioral changes.
When should I suspect a concussion has occured?
Following an injury and in the absence of the red flag symptoms above, a concussion should be suspected in the presence of any one or more of the following:
- Symptoms (such as headache, sensitivity to sound or light)
- Impaired brain function (e.g. confusion, difficulty with memory or feeling “foggy”)
- Physical signs (such as unsteadiness)
- Abnormal behavior (e.g. feeling nervous, emotional, irritable or sad)
How can I test an athlete if I think they have been concussed?*
You can use this online tool to assess your player's symptoms: https://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097506SCAT5.full.pdf.
In the event that the athlete is between the ages of 5 and 12 years of age, please use the following tool instead: http://bjsm.bmj.com/content/bjsports/51/11/862.full.pdf
*Note: assessment of an individual medical health status should be done by a trained, licensed health professional.
What kind of doctor should a concussed athlete see?
All concussed players should be seen by a physician and should fill out a Sports Concussion Assessment Tool 5 (SCAT5). If your family physician does not have you complete this test, ask them to refer you to a sports medicine physician. Consider one of the following clinics:
| Carleton University Sports Medicine Clinic |
| (613) 520-3510 |
| University of Ottawa Sports Medicine Clinic |
| (613) 564-3950 |
| CHEO Concussion Clinic |
| (613) 260-1477 x221 |
| Acquired Brain Injury (ABI) Outpatient Clinic - The Ottawa Hospital Rehabilitation Centre |
| (613) 737-7350 x 75406 |
How do I know if it’s safe to return to Ultimate?
Never return to play if you still have symptoms!
A player who returns to active play before full recovery from the first concussion is at high risk of sustaining another concussion, with symptoms that may be increased and prolonged. It is highly recommended that players be evaluated by a trained, healthcare professional and should be medically cleared to play if they have sustained or have had suspicion of sustaining a concussion.
Always follow the 6-Step Return to Play Guidelines.
6-Step Return to Play Guidelines
Step 1: No activity, only complete rest
Limit school, work and tasks requiring concentration. Refrain from physical activity until symptoms are gone. Once symptoms are gone, a physician, preferably one with experience managing concussions, should be consulted before beginning a step wise return to play process.
Step 2: Light aerobic exercise
Activities such as walking or stationary cycling. The player should be supervised by someone who can help monitor for symptoms and signs. No resistance training or weight lifting. The duration and intensity of the aerobic exercise can be gradually increased over time if no symptoms or signs return during the exercise or the next day.
- Symptoms? Return to rest until symptoms have resolved. If symptoms persist, consult a physician.
- No symptoms? Proceed to Step 3 the next day.
Step 3: Sports specific activities
Activities such as easy cutting or throwing can begin at step 3. There should be no body contact or other jarring motions such as high speed stops.
- Symptoms? Return to rest until symptoms have resolved. If symptoms persist, consult a physician.
- No symptoms? Proceed to Step 4 the next day.
Step 4: Begin drills without body contact
- Symptoms? Return to rest until symptoms have resolved. If symptoms persist, consult a physician.
- No symptoms? The time needed to progress from non-contact exercise will vary with the severity of the concussion and with the player. Proceed to Step 5 only after medical clearance.
Step 5: Begin drills with Body Contact
- Symptoms? Return to rest until symptoms have resolved. If symptoms persist, consult a physician.
- No symptoms? Proceed to Step 6 the next day.
Step 6: Game play











